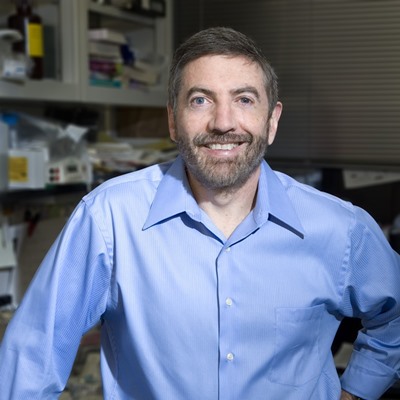

Ebru Erbay is an Assistant Professor in the Department of Molecular Biology and Genetics in Bilkent University in Ankara, Turkey since 2010 and Adjunct Professor in the Institute for Cardiovascular Prevention at the Ludwig Maximillians University in Munich, Germany since 2016. She received MD degree from Ankara University Faculty of Medicine and PhD in Cell and Structural Biology from the University of Illinois, Urbana-Champaign. Dr. Erbay completed her postdoctoral training with Prof. Gökhan Hotamışlıgil at Harvard University, School of Public Health. Dr. Erbay received many honors and awards including membership to the Turkish Academy of Science Young Investigator Program, EMBO Young Investigator Program, NIH’s Ruth Kirschstein Research Service Award, American Heart predoctoral fellowship, Proctor & Gamble thesis research award and graduated with high honors from Ankara University Medical School. During her PhD studies Dr. Erbay discovered the key role for a nutrient-sensitive mTOR pathway in myogenesis. As a postdoctoral fellow she demonstrated the causality of endoplasmic reticulum stress in macrophages to the development of atherosclerosis. Her current research focus is at the intersection of nutrient-sensitive, inflammatory and stress pathways in the context of metabolic diseases. Dr. Erbay is the first time recipient of the prestigious European Research Commission (ERC) Starting Grant in Life Sciences awarded to a researcher in Turkey. Her research program at Bilkent University is generously funded by additional grants from EMBO, European Commission, Turkey/Germany Bilateral Funding Scheme (TUBITAK/BMBF) and the International COST Action (TUBITAK). She also served an associate advisor to Science Translational Medicine.
Targeting Lipotoxic Endoplasmic Reticulum Stress in Cardiometabolic Syndrome
Cardiometabolic Syndrome (CMS) is profoundly influenced by pathways that lie at the interface of metabolism and inflammation. Metabolic overload initiates a chronic inflammatory response that promotes the complications of CMS. However, the molecular mechanisms linking metabolic stress to immune activation remain elusive. Earlier studies demonstrated that metabolic overload leads to stress in organelles, particularly in the endoplasmic reticulum (ER), and activates the unfolded protein response (UPR). The UPR is essentially an adaptive signaling emanating from the ER to cope with cellular stress and is important for cellular homoestasis. In addition to its protective role and stimulation of ER biogenesis, the UPR can also impinge on inflammatory signaling. Prolonged ER stress, however, is detrimental for cells and is shown to contribute to the pathogenesis of obesity, diabetes and atherosclerosis in part by activating pro-inflammatory and pro-apoptotic pathways. Moreover, the existence of inflammatory mediators, chemotactic cytokines, reactive oxygen species and other detrimental signals in obesity make it even more challenging for the ER to establish and maintain a healthy metabolic equilibrium. Clarifying the regulatory mechanisms and identifying novel, downstream players in a metabolically driven ER stress response is needed to develop specific and effective new therapeutic strategies for CMS. Our research group investigates the UPR that can sense the excess of nutrients and couple to inflammation, and whether its unique operation under metabolic stress can be suitable for therapeutic exploitation in CMS. Therefore, a major goal of my lab is to elucidate the molecular differences between metabolic ER stress and the adaptive UPR that could be therapeutically exploited in CMS. Our lab utilizes chemical-genetics coupled to proteomics to probe novel substrates of regulator kinases in the UPR. After validating these targets, we assess their contribution to inflammatory and metabolic processes as they relate to atherogenesis in vivo. Moreover, we use specific pharmacological inhibitors and genetic models to determine the contribution of individual UPR branches to atherosclerosis. I will present our progress with these novel mediators that may be developed into therapeutic targets in human atherosclerotic disease.